CONTACT US

Acne Treatments using the SharpLight’s AC415 nm Handpiece

Conducted by: Kipnis MD, A.M.L. Institute, Israel
Introduction
Acne is a chronic disease of the pilosebaceous follicle and is the most common skin disease, affecting up to 80% of individuals at some time in their life (Leyden).
Acne begins usually in adolescence, when hormonal changes cause the enlargement and then the obstruction of sebaceous glands in the skin. The obstruction of the gland opening causes the accumulation of sebum, which is followed by abnormal proliferation of the bacterial population, predominantly Propionibacterium acnes (P.acnes).
These pathophysiologic events result in the clinical expression of the painful, inflammatory pustules of acne. Not only can it cause disfigurement and permanent scarring, also have an adverse effect on psychological development, resulting in profound emotional scarring, which may lead to social phobias, withdrawal from society, clinical depression, and suicide (Cunliffe).
Topical acne medications are usually irritating to the skin and more than 40% of acne bacteria are insensitive to oral antibiotics. Therapy with Accutane is associated with possible severe side effects and is a costly and long treatment. Treatment time for responsive patients is usually at least three to four months.
Sun exposure is known to have some beneficial effects in up to 70% of patients with acne. Although solar or artificial UV light has a mild camouflage effect on acne, it’s comedogenic and photoaging effects diminish its use in acne therapy.
It is known that P. acnes produce porphyrin during their normal life cycle, as part of their normal metabolism process. Visible light in the blue range, or to a less extent in the red range, induces a photo destructive effect on Propionibacterium acnes that may take part in the decrease in acne severity during the summer.
A moderate decrease in the number of acne lesions was achieved previously by exposure to light sources that produce red light (Konig), mixed violet and ultra-violet (Meffert, Sigurdsson), or low intensity fluorescent light (blue and red).
This rapid growth in demand for aesthetic, light-based devices has led to substantial investment in the development of more effective and safer systems. Sharplight’s platforms are the result of such research and development efforts. This article summarizes Sharplight Medic’s experience with the Acne phototherapy using the AC415nm handpiece on the SharpLight’s platforms.
Materials and Methods
The system used for photoepilation was the Beamax intense pulsed light system with:
•Short pass filter of 415 nm (MAX acne hand piece)
• Spot size of 6.4 cm2
• Fluence range up to 8J/cm2
• Pulse durations of 30, 40, and 50 msec.
The SharpLight Max family IPL acne phototherapy is a drug-free modality for the treatment of mild and moderate inflammatory acne. A series of eight treatment sessions spaced over a period of one month is usually sufficient to reduce the number of papules and pustules by 60-65%. Patients undergoing the procedure enjoy shorter disease duration, reduced psychological stress and less likelihood for lesions to leave permanent scars.
Broad spectrum IPL phototherapy, available with the AC415 nm treatment handpiece, is based on three clinical mechanisms:
1. Visible light absorption in P.acnes produced porphyrin resulting in the release of singlet oxygen which destroys the bacteria.
2. Green to yellow light produce coagulation of blood vessels which feed the acne lesions.
3. Infrared heat which helps in drying up the lesion.
The SharpLight platform assures safety in applying acne phototherapy while the large spot size typically enables full face treatment in just a short 5-10 minute session.
A. Johnsson has found that the extruded contents of the sebaceous follicle yielded a spectrum with an excitation peak ranging from 381 to 405nm. This finding supports violet-blue light as an excellent wavelength range for destroying p.acnes. Other less absorptive wavelength was noted at – 504,576, 538 and 630nm.
Kjeldstad determined that shorter wavelength were more efficient for destroying the p.acnes, the expectation was in the range of 400 to 420nm, where the action spectrum showed a relative peak, (but not as high as UV).
All subjects completed a medical history form and were screened for any contraindications. They were briefed on the procedure, potential complications, and realistic expectations, and then signed an informed consent form.
For subjects under 18 years of age, a parent was asked to provide consent and sign the consent form.
Areas designated for treatment were then photographed. No topical anesthesia was applied.
A test was conducted to determine optimal treatment parameters for each patient. In most cases, the various skin types were treated as follows:
• Skin type I: Fluence range of 7-8 J/cm2 and pulse durations of 30 or 40 msec.
• Skin types II: Fluence range of 7-8J/cm2 and pulse durations of 30 or 40 msec.
• Skin types III: Fluence range of 6-7J/cm2 and pulse durations of 40 or 50 msec.
• Skin type IV-VI: Fluence range of 5-6J/cm2 and pulse duration of 50 msec.
This clinical review was conducted on 60 patients within the range of 16-24 years old with mild and moderate acne, at American Laser clinics in Rishon le Zion, Israel, April to September 2006.
Side effects of the treatment, such as pain or excessive erythema, as well as any adverse effects, such as skin burns, hypo/hyper pigmentation, excessive swelling or induced hair growth, were not recorded. The subjective overall assessment grade of the physician was reported on table 1 below.
Patients were treated two times a week for a total of 8 session treatments, and were followed up 1-3 months after the last procedure. Treatment required 20 minutes for full face treatment.
Two passes with shorter pulse duration was applied when small an amount of comodones were noted.
Results
Acne is a multifactorial process involving high sebum excretion rates resulting from the glands’ response to androgens, comedone formation, and colonization of the gland with P. acnes and production of chemo-attractant cytokines for leucocytes. There is a correlation between the reduction in numbers of P. acnes and specified wavelength treatment modality in this clinical review, showing improvement in patients with acne.
These porphyrins mainly absorb visible light at 400-415 nm. In-vitro studies have shown that irradiation of P. acnes colonies with blue visible light leads to photoexcitation of the bacterial porphyrin stimulating singlet oxygen production and destruction of P. acnes. Light absorption by target cells also induces changes in membrane permeability leading to proton influx and dissipation of pH gradients across the cell membrane.
Changes in pH gradients inhibit the proliferation of P. acnes, the causative organism of inflammatory processes. Light absorbed by photo acceptors combined with short-term changes of redox potential provokes mitogenic signals in cells and stimulates cellular respiration and proliferation. These factors could play a significant part in the post treatment healing of inflamed acne skin, stimulating natural repair mechanisms. In this study we have been able to demonstrate that blue light therapy using 415 nm significantly reduces inflammatory acne lesions.
The average single and multiple sessions’ treatment results on various anatomical sites and subject’s gender are summarized in Table.1.
The number of treatment sessions required to achieve final results was eight; all patients could comfortably bear the treatment pain or were not significantly affected by a feeling of pain. No adverse effects were recorded in this series of treatments apart from light sensation of heat. Of the 60 patients treated (37) were very satisfied with the results, (11) were satisfied with the results and the (12) remaining didn’t notice any significant changes. No significant difference was noted between male and female patients. See fig 1/2-1/4
Table 1. Physician assessment
| Body Part Treated | 1st Treatment clearance | Final Result in % | 1 month post last procedure | 3 month post last procedure |
| Face | 15% | 62% | same | A�same |
| Upper Back | 12% | 55% | same | same |
| Shoulder | 15% | 50% | same | A�same |
Conclusions
Our initial experience with the AC415nm application, as reported in the above chart, demonstrates the physiciana’s overall assessment report.
This chart has similar results to parallel light-based systems.
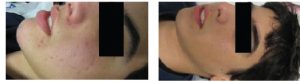
Figure 1 and 2 shows the results of acne clearance from the first procedure to the last of eight procedures, and up to three months after the last procedure.
Figure 1. Average clearance of non infamatory acne lesions
Figure 1/2. Results of acne clearance (Three Months after Last Procedure)
With the courtesy of :
Ms. Rachel Zohar P.M.E.C. / Beautician,
Private Clinic Haifa ISRAEL
Before After
Figure 1/3. Results of acne clearance (Three Months after Last Procedure)
With the courtesy of:|
Ms. Rima Aboui P.M.E.C. / Beautician
Private Clinic Nazareth ISRAEL
Before After
Figure 1/4. Results of acne clearance (Three Months after Last Procedure)
With the courtesy of :
Ms. Rachel Zohar P.M.E.C. / Beautician
Private Clinic Haifa ISRAEL
Before After
References
1. Jowett S, Ryan T. Skin disease and handicap: an analysis of the impact of skin conditions. Soc Sci Med 1985; 20 (4): 425-9
2. Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol 1998; 139 (5): 846-50
3. Cotterill JA, Cunliffe WJ. Suicide in dermatological patients. Br J Dermatol 1997; 137 (2): 246-50
4. Norris JF, Cunliffe WJ. A histological and immunocytochemical study of early acne lesions. Br J Dermatol 1988; 118 (5): 651-9
5. Mouser PE, Baker BS, Seaton ED, et al. Propionibacterium acnes reactive T-cell lines established from early inflamed acne lesions [abstract]. J Invest Dermatol 2001; 117: 803
6. Leyden JJ, McGinley KJ, Mills OH, et al. Propionibacterium levels in patients with and without acne vulgaris. J Invest Dermatol 1975; 65 (4): 382-4
7. Melo TB. Uptake of protoporphyrin and violet light photodestruction of Propionibacterium acnes. Z Naturforsch [C] 1987; 42 (1-2): 123-8
8. Lee WL, Shalita AR, Poh-Fitzpatrick MB. Comparative studies of porphyrin production in Propionibacterium acnes and Propionibacterium granulosum. Bacteriol 1978; 133 (2): 811-5
9. Konig K, Ruck A, Schneckenburger H. Fluorescence detection and photodynamic activity of endogenous protoporphyrin in human skin. Optical Engineering1992; 31(7):1470-1474.
10. Kjeldstad B, Johnsson A. An action spectrum for blue and near UV inactivation Propionibacterium acnes; with emphasis on a possible porphyrin photosensitization. Photochem Photobiol 1986; 43 (1): 67-70
11. Byrne PA, Williams BD, Pritchard MH. Minocycline-related lupus. Br J Rheuafter matol 1994; 33 (7): 674-6
12. Combination blue (415 nm) and red (633 nm) LED phototherapy in the treatment of mild to severe acne vulgaris.Authors: Goldberg, David1; Russell, Bruce1Source: journal of cosmetic and laser therapy – Volume 8, Number 2, June 2006, pp. 71-75(5)